
October • 12 • 2023
Nursing Peer Review: Quality Improvement Through Shared Learning
Summary
The peer review process is intended to improve patient safety and support a continuous learning culture – shifting the focus from identifying persons responsible for an adverse event to understanding the organizational systems that contribute to unanticipated outcomes.
Peer review is a process whereby healthcare professionals evaluate the quality of their colleagues’ work to ensure it meets the prevailing professional standards of care. This nonpunitive process is intended to improve patient safety and support a continuous learning culture. The peer review process shifts the focus from identifying persons responsible for an adverse event to understanding the organizational systems that contribute to unanticipated outcomes.
Physician peer review began in the early 20th century as a method of defining standard of care requirements for hospitals and their medical staffs. Today, physician peer review is a mandatory process that occurs in all U.S. hospitals. First defined by the American Nurses Association in 1988, the nursing peer review processes is comparatively new and much less widespread. Its intent mirrors that of physician peer review—to ensure that well-recognized standards of care are met and to apply lessons learned to improve patient care quality and safety. Recent data analysis reveals that the delivery of nursing care has room for improvement.
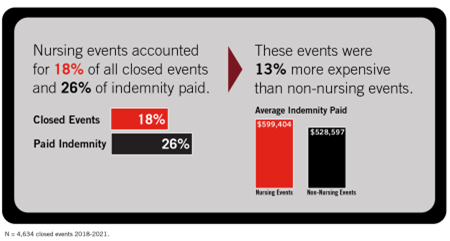
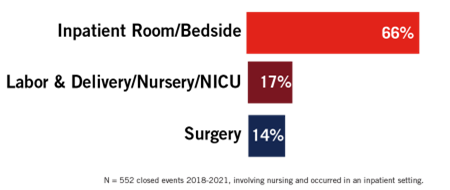
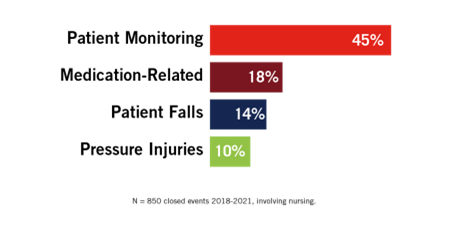
Coverys’ analysis of 4,634 claims that closed between 2018 and 2021 identified 850 events in which nurses were directly involved in care that resulted in the alleged medical error. This data provides valuable “signals” that lend insight into existing vulnerabilities and guide organizations in implementing proactive risk and quality improvement strategies. Here is what this data reveals:
Nursing events can be expensive.
Most of the identified nursing events occurred in the inpatient setting.
Almost half of the identified nursing events involved patient monitoring.
Meaningful nursing peer review can enhance patient safety, improve quality of care, and support a culture of continuous learning. The American Nurses Credentialing Center (ANCC) has identified numerous standards consistent with the highest quality of nursing care and healthcare organizational structure. According to the ANCC, “The peer review process stimulates professionalism through increased accountability and promotes self-regulation of the practice.” Despite the benefits, adoption of nursing peer review across healthcare remains limited.
Risk Recommendations
Nursing peer review can be a powerful quality improvement and patient safety tool when implemented in an organization that embraces nonpunitive, just culture principles. The peer review structure allows nursing errors and adverse events to become learning opportunities to improve and enhance patient safety. Consider the following when implementing your organization’s nursing peer review program:
- Do your homework. Research the nursing peer review process and the ways it can benefit your organization. Seek nursing peer review policies and procedures from reputable sources. Assess multiple nursing peer review programs/models at other facilities and utilize the practices that will work best at your own organization. Share your key learnings with the governing body, leadership, and other thought leaders in your organization.
- Assess organizational capacity. Like physician peer review programs, nursing peer review programs require an investment of financial and human resources. The nursing peer review program must be staffed by adequate numbers of highly trained and/or experienced employees and peer review committee members. The cost of acquiring, creating, and maintaining documents related to the nursing peer review processes should be factored into the program budget. Work with an interdisciplinary team to determine whether your organization has the resources, capacity, and ability to build and support a nursing peer review program.
- Know the law. Consult an attorney to understand the legal protections your state affords to nursing peer review and how to optimize them. Work with your attorney to ensure the proper design and implementation of a nursing peer review program and process that comply with state and federal law. Confirm that all documents related to the peer review process contain sufficient language to maximize the protections afforded under relevant state law.
- Map a process. Plan the implementation of a nursing peer review process that:
- Provides guidelines for case submittal.
- Identifies triggers for peer review and appropriate reviewers.
- Creates a charter to document the intent and actions of the clinical peer review committee.
- Selects a committed and diverse clinical peer review committee membership.
- Maintains accurate records and designates where to keep them.
- Maintains confidentiality of all process phases and documentation.
- Creates a written nursing peer review policy and procedure.
- Implement the plan. After the plan is finalized and approved, implement the nursing peer review program as planned. Encourage staff buy-in by educating them about the purpose, value, and process of nursing peer review. Ensure that all involved nursing staff are aware of their respective roles and responsibilities. Notify all involved staff of the program’s start date.
- Evaluate regularly. Identify quantifiable measures to track program progress/success. Share data and responsive actions with the appropriate quality improvement and/or patient safety committee to facilitate process improvement. Regularly review and evaluate the program and make improvements as necessary.
Additional Resources
- Peer Review Tip: Distinguishing the Difference Between Peer Review, Peer Evaluation, and Peer Feedback
- American Nurses Association, Stepping up Professional Practice: Implementing Nursing Peer Review
- Coverys Risk Management Brief, Peer Review: Overview and Process
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.