
Summary
Medication error is one of the leading causes of avoidable harm in healthcare organizations worldwide. While developing a strong medication safety program is a multidisciplinary effort, the responsibility for safe administration of medications largely falls on the shoulders of nurses.
Medication error is one of the leading causes of avoidable harm in healthcare organizations worldwide. When in 2017 the World Health Organization (WHO) launched its third Global Patient Safety Challenge, "Medication Without Harm," it called for action from healthcare practitioners and organizations to reduce patient harm related to medication error.
On September 17, WHO will reaffirm its commitment to this challenge when it celebrates World Patient Safety Day with the “Medication Without Harm” slogan. Each year, medication errors lead to thousands of deaths and hundreds of thousands of injuries in the U.S. alone. The cost associated with caring for patients injured by medication error exceeds $40 billion per year.
Not only are medication errors detrimental to the well-being of the patient, often resulting in serious injury, disability, or death, they can impact the financial well-being of a healthcare organization. Because the Centers for Medicare & Medicaid Services does not reimburse for certain hospital-acquired injuries, including injuries related to medication error, these events can significantly reduce the ever-shrinking revenue stream of healthcare organizations. Recent news stories have ignited heated discussion about how the potential for criminal exposure related to medication error will affect patient safety efforts and the nursing profession.
While developing a strong medication safety program is a multidisciplinary effort, the responsibility for safe administration of medications largely falls on the shoulders of nurses. The Bureau of Labor Statistics estimates that 194,500 nurse job openings will be created annually over the next decade. As the number of nurses in the workforce shrinks, staffing shortages will likely reduce the ability of healthcare organizations to deliver consistent, quality patient care. One key area of vulnerability that may be impacted by the nursing shortage is medication error—a risk that is directly correlated to nursing vigilance, monitoring, and intervention.
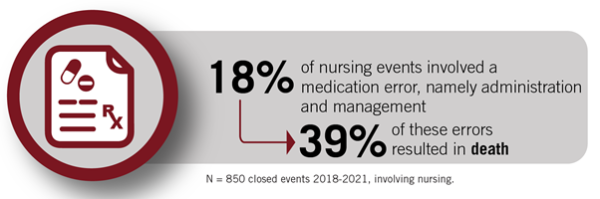
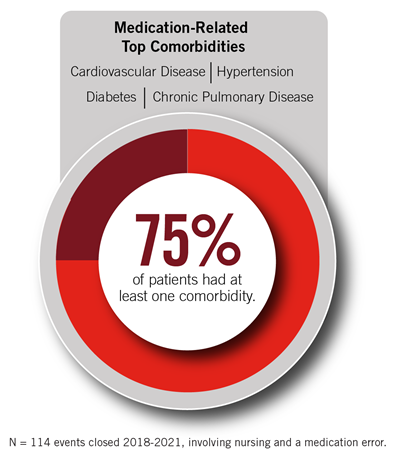
Coverys has analyzed closed claims data to better understand the factors contributing to medication error and the effect those errors have on our policyholders. These data provide valuable signals that can lend insight into existing vulnerabilities and help policyholders implement proactive risk strategies. Coverys examined 4,634 events that closed between 2018 and 2021 and identified 850 specific events directly involving registered, licensed practical, or student nurses. There were 114 events involving nursing and a medication error. Below are some key insights gleaned from these data:
Organizations can prevent many medication errors by implementing and consistently adhering to a medication safety program. A well-designed medication safety program requires a multidisciplinary approach, optimization of electronic health record (EHR) capabilities, standardization, continuous performance improvement efforts, and, most of all, a just culture that encourages open reporting of errors and near misses. Consider the following when implementing or reviewing your organization’s medication safety program:
- Develop an organizationwide medication safety plan. Your medication safety plan should establish measurable annual goals. Ensure that the plan reflects best practices described by patient safety organizations such as the Institute for Healthcare Improvement, the Institute for Safe Medication Practices, and accreditation bodies. Implement patient safety interventions, including a bar-coded medication administration system, standardized order sets, two patient identifiers, and management of high-alert and look-alike/sound-alike medications.
- Leverage technology. Enlist a multidisciplinary team to optimize use of electronic medication safety features and equipment by reconfiguring medication dispensing cabinets to require input of at least the first five letters of a drug name and requiring generic names to be used when ordering medications. Educate nursing and medical staff on the importance of knowing how to use the following technological safety features:
- EHR medication safety (drug interactions, dosing alerts, allergies, etc.).
- Computerized provider order entry.
- Smart pumps with hard dosing limits.
- Standardized dosing/orders for high-risk medications.
- Bar code technology at bedside.
- Capnography with opiates via patient-controlled analgesia.
- Enhance the medication reconciliation process. Develop a process to ensure that the registered nurse obtains and documents a complete medication assessment upon admission and at all points of care transition, including discharge. Ensure the medication history and reconciliation includes:
- Current medications/dosages/frequency.
- Route and time of last dose.
- Over-the-counter meds, including herbal and nutritional supplements, vitamins, etc.
- Illicit drug, marijuana, and cannabidiol use.
- Allergies and allergic response.
- A review by a licensed pharmacist.
- Educate nursing staff. Require medication competency training for new nurses that includes medication safety principles, dosing calculations, safe IV injection practices, occurrence reporting, and organizational processes and technological systems in place to support safe medication management. Implement continuous education for nursing staff that includes training on new medications prior to their availability on the unit, high-alert and infrequently used medications, medication delivery system changes, and medication reconciliation. Develop hands-on competencies for high-risk medications on each unit, as applicable. Conduct annual medication competencies for nurses and document completion in personnel files.
- Minimize distraction and interruption. Medication preparation and administration are nursing activities that require focus and concentration. Studies have shown that minimizing interruptions during the medication administration process significantly reduces errors. Develop a process that discourages interruption while nurses are administering medication and empower nurses to delay interruptions without fear of repercussion. Educate staff about the link between interruption and medical error so they understand why they are being asked to return later. Explore whether controllable environmental issues like workload, equipment design, or IT systems may be inadvertently generating distractions and interruptions.
- Report and monitor medication errors. Educate all staff on how occurrence reporting aids in identifying medication errors and near misses. Utilize patient safety culture principles, shared accountability, and other incentives to enhance reporting. Ensure that an appropriate nursing quality committee or patient safety/medication safety committee routinely reviews and acts on identified medication safety issues. Conduct a failure mode and effects analysis on high-risk medication delivery processes to proactively identify risk reduction methods. Conduct medication safety audits on each unit to identify opportunities for improvement, including the use of workarounds to bypass safety mechanisms.
- Educate patients, families, and caregivers. Engage staff pharmacists when managing medications for patients who are on numerous or uncommon medications or have multiple comorbidities. When discharging a patient with multiple new medications, consider having a pharmacist prepare the medication discharge instructions. Develop a formal process for educating patients and their families about medications. Look for patient education documentation when conducting focused medical record audits.
Additional resources:
- PSNet: Medication Administration Errors
- RaDonda Vaught, medication safety, and the profession of pharmacy: Steps to improve safety and ensure justice.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.