
February • 29 • 2024
Managing Risk When Dealing With Biased Patient Requests
Summary
Biased patient demands are not uncommon. Healthcare facilities must establish procedures to help staff members manage bias incidents.
In recent years, healthcare facilities have given considerable attention to the issue of provider bias – and for good reason. Cognitive bias has a direct correlation to diagnostic error and has been identified as a contributor to sentinel events. However, patients may also be biased and cause harm. Biased attitudes directed at healthcare workers are often expressed via overtly negative comments, such as microaggressions. Allowing microaggressions and complying with biased patient demands may contribute to healthcare worker moral distress, psychological harm, and burnout. Healthcare organizations need a response strategy that mitigates these risks.
The U.S. Workforce Is Becoming More Diverse
The U.S. workforce has become more diverse in terms of gender, race, ethnicity, and even age as more women and immigrants have entered the workforce and workers have delayed retirement. Notably, Gallup says the average retirement age has increased from 57 in the 1990s to 61 today, whereas the U.S. Bureau of Labor Statistics (BLS) says foreign-born workers now account for 18.1% of the civilian workforce. KFF says 40% of healthcare workers are people of color.
Patient Requests Rooted in Bias
Patients may be biased against providers based on age, gender, race, religion, ethnicity, or country of origin. Furthermore, they may be biased against providers with characteristics that are similar or different to their own. For example, male patients may be biased against female doctors, but female patients may also be biased against female doctors.
Patients may make demands related to their biases, such as requesting a provider of a different gender, race, ethnicity, or religion.
Reasonable vs. Unreasonable Requests
In an article published in the ASCO Post, Thaddeus Mason Pope, JD, PhD, points out that some requests that seem discriminatory may not actually be rooted in bigotry – they may stem from religious convictions, a desire to be modest, or a reaction to past trauma. Further compassionate inquiry may help healthcare workers find the root of the patient’s request. Accommodating reasonable requests when possible can benefit the patient’s satisfaction and health outcome.
Such accommodation may be permissible under federal anti-discrimination laws when the person’s gender, race, or other protected class is relevant to the services being provided, such as physical examinations under clothing. However, nonviolent misconduct appearing as biased requests that are rooted in racism, sexism, ageism, etc., must be immediately addressed. Accommodation of these requests may not only harm providers, but also expose organizations to lawsuits.
Responding to Biased Requests
A response to biased patient requests should:
- Comply with regulations.
- Be based on organizational policies.
- Be effective and consistent.
To understand why this is critical, consider the following case study. An infant’s father demanded that no Black nurses touch his child. To communicate this to staff, a sign is placed in the NICU stating that no Black staff may treat the patient. This opened the hospital to allegations that it violated the First and Fourteenth Amendments to the U.S. Constitution, equal protection laws, and state-based anti-discrimination legislation. The hospital’s reaction also allegedly contributed to employee dissatisfaction, disengagement, and burnout.
The Mayo Clinic’s SAFER Model
Since biased comments and requests may catch healthcare workers off guard, it’s useful to have a prepared response and/or scripting. Healthcare workers should be encouraged and empowered to consider the patient’s request with curiosity over judgment. Repeating the patient’s request may cause the patient to self-correct. If the patient insists, the use of empathetic listening and standard respectful responses may be helpful to keep the lines of communication open and maintain a trusting relationship. For example, suggest standard responses such as “Please help me understand your request” or “We are here to help you as a team. We do not change doctors/nurses/etc., due to their race/ethnicity/religion/etc.” The former may be ideal when the reason for the request is unclear and may be reasonable, whereas the latter is a response to bigoted requests.
The Mayo Clinic’s SAFER model provides a five-step approach to deal with a biased response:
- Step in when you observe behavior that does not align with your organization’s values.
- Address the inappropriate behavior with the patient or visitor.
- Focus on your organization’s values (such as respect and healing).
- Explain your organization’s expectations and set boundaries with patients and visitors.
- Report the event to your supervisor and document the incident.
A decision tree can be useful to help determine when to grant, deny, or report a biased request. The decision tree, developed by the Mayo Clinic, is a good example as it considers several important factors to aid in decision-making. For example, if the patient’s condition is emergent or their mental state unstable, it may be necessary to grant the request for safety reasons. If the patient’s condition is not emergent, but their health may deteriorate if the request is not granted, it may be necessary to grant the request. However, if the request is inappropriate and their condition is stable, employees should deny a biased request.
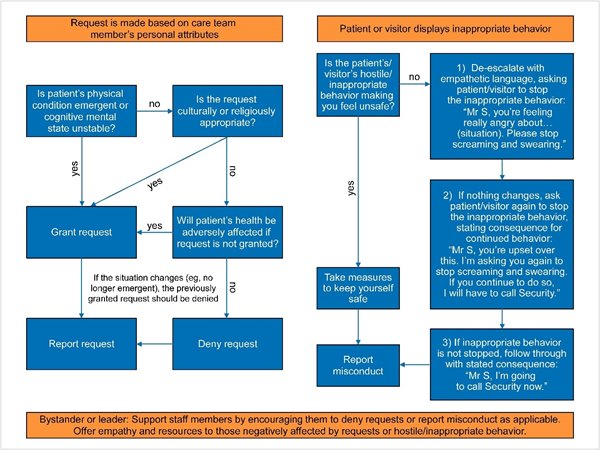
Source: Mayo Clinic’s 5-Step Policy for Responding to Bias Incidents, published in the AMA Journal of Ethics
In Conclusion
Biased patient requests are an unfortunate reality for many healthcare workers. Healthcare organizations should develop policies in collaboration with legal and risk management to protect workers and reduce exposure to claims of discrimination. When incidents occur, employees should respond in accordance with the policy and carefully document their decision-making process and conversations.
Healthcare facilities should also consider their response to biased demands comparably to their response to nonviolent misconduct or passive workplace violence. The skillful use of de-escalation strategies, described in this Coveys blog, may not always be necessary, however, they may become essential if the patient becomes agitated or unreasonable.
Finally, healthcare leaders should foster a welcoming environment to ensure emotional safety for healthcare workers to discuss incidents of discrimination. It is helpful to hold practice drills, have scripts at the ready for difficult conversations, and offer de-escalation training and access to emotional support services for all employees. Be prepared to demonstrate why, in healthcare, the customer is not always right.
This article is based in part on a Coverys presentation “Healthcare’s Response to Patients’ Biased Demands,” presented by Jenelle Arnao, DHS, MS, CPHRM, Senior Risk Consultant at Coverys.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.