
View Expert Insights
April • 20 • 2023
Healthcare Risk Data Strategy: Your Key to Improving Patient Outcomes
Article
Summary
Leverage risk data in healthcare to develop proactive strategies that lower insurance costs while improving patient safety and outcomes.
Does your organization have a healthcare data strategy? While many risk managers want to leverage data to better understand and mitigate risk, it’s an initiative that is sometimes deprioritized when other crises arise. However, if patient safety is a priority, data analysis should rise to the top of your list. With a better understanding of your organization’s healthcare data, you can drive proactive risk management practices that improve patient outcomes and support patient safety programming, while also reducing insurance and litigation costs.
As analytics and artificial intelligence capabilities have developed, data has received significant attention. Although data has enormous potential, it’s important to understand its limits. It is easy to confuse data with knowledge, but the two are not the same. Alone, data is one piece of information connected to a time and place. To understand what it means, and the story it may tell, context is critical.
For example, imagine a unit had 10 falls in January and five falls in February. Does this data prove the unit has become 50% better at preventing falls? No. To draw such conclusions, it would be necessary to address other factors that could impact the figures, such as whether falls were underreported or if the unit had fewer or lower acuity patients during the second month.
In addition to the context, it’s important to consider both the source and delivery of data. There are an incredible number of data sources that you can mine and source. Knowing which ones are best options can be very difficult because you want your data to be meaningful. And being meaningful directly relates to your audience. People want to connect with data. Considering what your audience needs to know can help lead you to the sources that will provide the most meaningful insights. Break the data up into pieces to help your audience understand why it is meaningful.
Claims data – like all types of data – has limitations. The number of instances tends to be small, the data always refers to the past, and unique convergences of factors may not repeat themselves in the same way.
Despite these limitations, claims data can provide signals about where to focus some risk management and patient safety efforts. Some of the signals you can glean from this data may be weak and represent anomalies. Other signals may be moderate or strong, such as highlighting concerns in your culture of safety and decreased psychological safety. By identifying what happened in the past, it is possible to determine whether the same factors continue to undermine patient safety.
A practice’s claims data can reveal a tremendous amount of actionable information. The key is to break the data down into smaller chunks of information that can provide answers to critical questions, such as:
In addition to malpractice, risk data in healthcare can come from multiple sources. Some of the most critical sources of data include:
Data captures past events, but risk managers need insights into present and future risks. Through predictive scoring, you can transform past data into actionable insights.
Predictive scoring provides insight about the probability of future events. Risks managers can use the same insights to identify and mitigate risk. Here are three key questions to ask:
A value-based model to support better outcomes involves four steps:
1. Signals. Capture the deeply-rooted drivers of malpractice cases. Aggregated comparisons can provide context.
2. Assessment. This involves risk management and advanced analytics. Identify the signals and determine how strong they are. Establish whether the vulnerabilities still exist and what risk will exist if you do not take action.
3. Implementation. Implement solutions designed to reduce risks and maximize reimbursements.
4. Improve Outcomes. Measure the results to determine how outcomes have improved. Risk managers should see reduced malpractice risk, improved revenue, safer care, and thriving providers and healthcare facilities.
When leveraged effectively, data can yield insights into present and future risks. Healthcare risk managers can use risk data to develop proactive strategies. These data-backed risk control measures have the potential not only to lower insurance costs but also to improve patient safety and outcomes.
This article is based in part on “Risk Management Data: Developing Meaningful Data to Tell Your Story,” presented to the American Society for Health Care Risk Management by Robert Hanscom, Collin Wedel, Natalie Kaiser, and Josh Hyatt.
Data Is Not Knowledge
As analytics and artificial intelligence capabilities have developed, data has received significant attention. Although data has enormous potential, it’s important to understand its limits. It is easy to confuse data with knowledge, but the two are not the same. Alone, data is one piece of information connected to a time and place. To understand what it means, and the story it may tell, context is critical.For example, imagine a unit had 10 falls in January and five falls in February. Does this data prove the unit has become 50% better at preventing falls? No. To draw such conclusions, it would be necessary to address other factors that could impact the figures, such as whether falls were underreported or if the unit had fewer or lower acuity patients during the second month.
In addition to the context, it’s important to consider both the source and delivery of data. There are an incredible number of data sources that you can mine and source. Knowing which ones are best options can be very difficult because you want your data to be meaningful. And being meaningful directly relates to your audience. People want to connect with data. Considering what your audience needs to know can help lead you to the sources that will provide the most meaningful insights. Break the data up into pieces to help your audience understand why it is meaningful.
Claims Data Is Just One Type of Risk Data
Claims data – like all types of data – has limitations. The number of instances tends to be small, the data always refers to the past, and unique convergences of factors may not repeat themselves in the same way.Despite these limitations, claims data can provide signals about where to focus some risk management and patient safety efforts. Some of the signals you can glean from this data may be weak and represent anomalies. Other signals may be moderate or strong, such as highlighting concerns in your culture of safety and decreased psychological safety. By identifying what happened in the past, it is possible to determine whether the same factors continue to undermine patient safety.
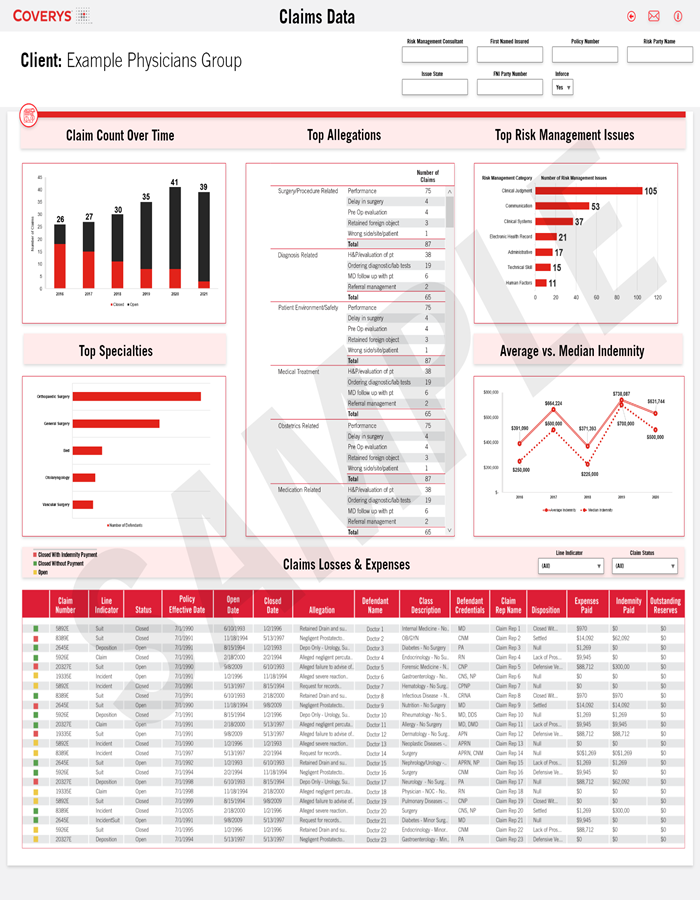
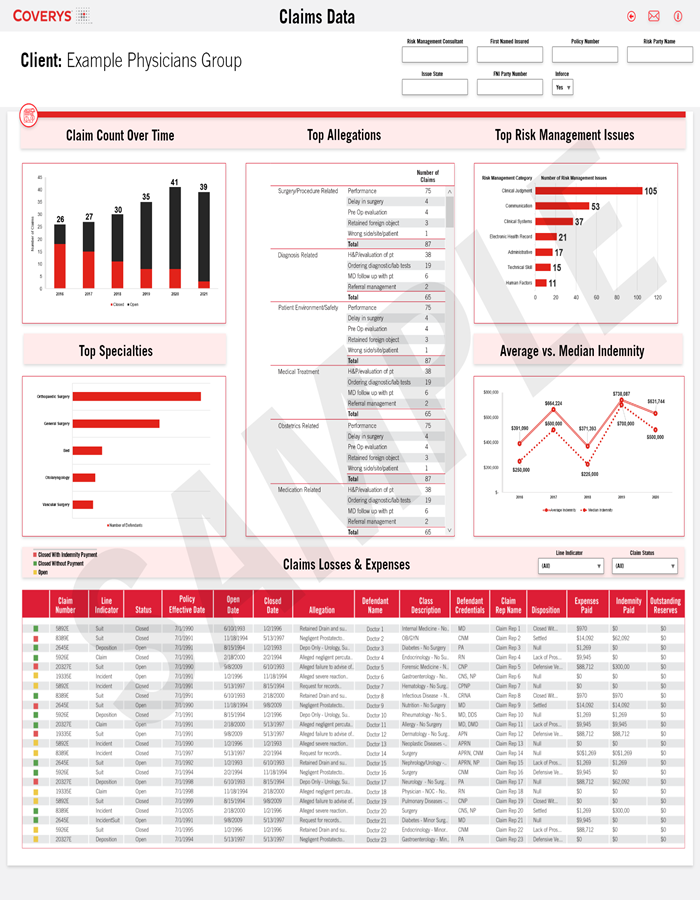
A practice’s claims data can reveal a tremendous amount of actionable information. The key is to break the data down into smaller chunks of information that can provide answers to critical questions, such as:
- How has claims frequency changed over time? Although other factors (for example, patient load) can impact claims frequency, knowing whether the claim count is increasing or decreasing may tell you whether risk management is improving.
- What are the top allegations? For example, are the majority of claims related to diagnosis or are you seeing more claims related to procedures? By identifying the most common complaints and their sources, you can prioritize areas for focus.
- What are the top risk management issues? For example, do claims stem from challenges related to technology or are they more often a result of human error or miscommunication? These insights can help you pinpoint the underlying causes.
Other Data Sources
In addition to malpractice, risk data in healthcare can come from multiple sources. Some of the most critical sources of data include:
- Patient complaints.
- Patient satisfaction surveys.
- Adverse event data.
- Root cause analyses (for serious reportable events).
- Morbidity and mortality rounds.
- Patient rounds.
- “Near-miss” data (from events that did not lead to claims but may point to underlying factors that could lead to claims).
- Credentialing and privileging reviews.
- Culture of Safety surveys.
- Pharmacy and therapeutics investigations.
- Regulatory and accreditation survey results.
- Failure Mode Effects Analysis results.
- And many more.
Leveraging Predictive Scoring
Data captures past events, but risk managers need insights into present and future risks. Through predictive scoring, you can transform past data into actionable insights.Predictive scoring provides insight about the probability of future events. Risks managers can use the same insights to identify and mitigate risk. Here are three key questions to ask:
- What is the probability of a future claim in the next three years? This indicates how serious the risk is.
- What percentage of providers in the same category have had a claim in a three-year period? This provides a benchmark comparison to reveal whether your risk is higher or lower than average.
- What are the key factors contributing to the predictive score? This lets you know the root causes – i.e., the issues you need to address to mitigate risks.
From Data to Outcomes
A value-based model to support better outcomes involves four steps:1. Signals. Capture the deeply-rooted drivers of malpractice cases. Aggregated comparisons can provide context.
2. Assessment. This involves risk management and advanced analytics. Identify the signals and determine how strong they are. Establish whether the vulnerabilities still exist and what risk will exist if you do not take action.
3. Implementation. Implement solutions designed to reduce risks and maximize reimbursements.
4. Improve Outcomes. Measure the results to determine how outcomes have improved. Risk managers should see reduced malpractice risk, improved revenue, safer care, and thriving providers and healthcare facilities.
Improving Patient Safety While Lowering Costs
When leveraged effectively, data can yield insights into present and future risks. Healthcare risk managers can use risk data to develop proactive strategies. These data-backed risk control measures have the potential not only to lower insurance costs but also to improve patient safety and outcomes.This article is based in part on “Risk Management Data: Developing Meaningful Data to Tell Your Story,” presented to the American Society for Health Care Risk Management by Robert Hanscom, Collin Wedel, Natalie Kaiser, and Josh Hyatt.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.