Summary
Understanding the factors that give rise to dental claims can provide insight to practice managers and help them implement proactive risk management strategies to enhance patient safety and reduce claims.
Professional liability claims can be disruptive and stressful for dental practitioners and their staff. Understanding the factors that give rise to dental claims can provide insight to practice managers and help them implement proactive risk management strategies to enhance patient safety and reduce claims.
A 57-year-old patient visited the dental office for an extraction of three teeth with bone grafting under moderate sedation. During the procedure, the patient received multiple sedative medications, including nitrous oxide. As the final extraction began, the patient became apneic, and her oxygen saturation dropped to 50%. 911 was called, and the procedure was stopped. When the patient’s oxygen saturation improved slightly, the dentist cancelled the call to 911, and the procedure was continued despite staff member requests to stop the procedure and stabilize the patient.
The patient filed a lawsuit against the dentist alleging cognitive impairment from the hypoxic event. In her deposition, the patient testified that she had advised the dentist of her obstructive sleep apnea (OSA) history during her preprocedure appointment. The dentist denied this conversation took place. Documentation of the patient’s complete medical history did not appear in the dental record.
Dental experts testified that the dentist acted below the standard of care by:
Case Summary
A 57-year-old patient visited the dental office for an extraction of three teeth with bone grafting under moderate sedation. During the procedure, the patient received multiple sedative medications, including nitrous oxide. As the final extraction began, the patient became apneic, and her oxygen saturation dropped to 50%. 911 was called, and the procedure was stopped. When the patient’s oxygen saturation improved slightly, the dentist cancelled the call to 911, and the procedure was continued despite staff member requests to stop the procedure and stabilize the patient.The patient filed a lawsuit against the dentist alleging cognitive impairment from the hypoxic event. In her deposition, the patient testified that she had advised the dentist of her obstructive sleep apnea (OSA) history during her preprocedure appointment. The dentist denied this conversation took place. Documentation of the patient’s complete medical history did not appear in the dental record.
Dental experts testified that the dentist acted below the standard of care by:
- Failing to get a complete medical history or ignoring the patient’s OSA history.
- Administering moderate sedation without proper monitoring or management.
- Administering high doses of sedative medications without properly titrating the medications.
Dental Claims Data
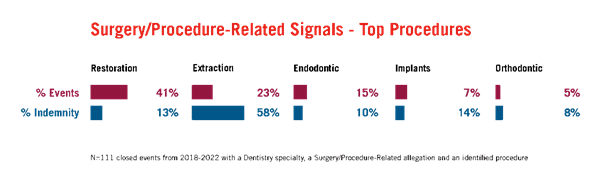
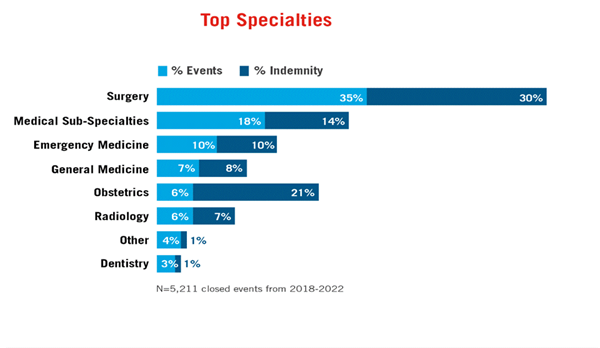
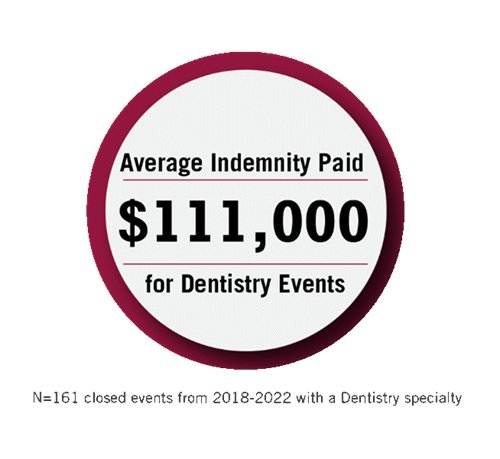
Coverys has analyzed closed dental events to better understand the factors contributing to dental claims and the impact those claims have on dental practices. While this data is not absolute, it provides valuable signals that can lend insight into existing vulnerabilities and allow dental practitioners and practices to implement proactive risk strategies. For this article, Coverys analyzed 5,211 closed events from 2018-2022 and identified 161 events that were associated with dentistry. This data further reveals:
Compared to other clinical specialties, dental events do not occur often.
But when dental events occur, they can be expensive.
Restorations and extractions are responsible for most dental events.
Risk Management Recommendations
Unexpected complications from even routine procedures like restorations and extractions can result in adverse outcomes, especially if the patient’s existing health issues are not considered. Proactive risk management strategies help prevent claims and enhance patient safety. Consider the following when assessing your practice for risk vulnerabilities:- Obtain a thorough health history. Update the patient’s health history during each visit, especially during preoperative visits. Include in the health history the patient’s complete medical, dental, and surgical history along with their current prescriptions, over-the-counter medications, and supplements. During each visit, verify with the patient any medication allergies and/or an intolerance history and document this in a prominent location in the dental record. Allow time during each visit for the dentist to review and discuss the patient’s health history with them prior to performing any procedure. Document the patient’s health history thoroughly in the dental record.
- Obtain informed consent. Inform the patient of the risks, benefits, and alternatives to the proposed treatment and obtain their written consent to proceed. Document the informed consent discussion in the dental record. Be sure to include a copy of the signed consent form in the designated portion of the dental record.
- Perform a complete preprocedure assessment. Conduct a thorough preoperative assessment to determine if the patient is a candidate for office surgery or requires a hospital-based procedure. This may include an anesthesia assessment, X-rays, lab testing, and medical clearance from other practitioners when indicated. Conduct a pre-anesthesia evaluation to determine a patient’s eligibility and safety for receiving moderate or deep sedation, or general anesthesia. Refer patients to an appropriate specialist when indicated.
- Refine anesthesia policies and procedures. Develop evidence-based policies and procedures that reflect state requirements and best practices for anesthesia administration. Include in policies and procedures a requirement for continuous monitoring when administering moderate or deep sedation, or general anesthesia. Ensure that dental practitioners keep abreast of current information on anesthetic drugs, administration methods, and dosages.
- Prepare for emergencies. Although rare, medical emergencies happen, and good preparation can impact outcomes. Develop a written plan that specifically instructs staff what to do in the event of a medical emergency. Make sure age-appropriate emergency equipment, supplies, and medications are immediately available. Ensure the plan includes criteria and procedures for hospital transfer. All dentists and staff with patient care responsibilities should be certified in basic life support. Dentists who administer deep or moderate sedation and their participating staff should be certified in advanced cardiac life support.
- Confirm that dentists and staff are properly trained. Ensure that dentists and staff are performing duties within their defined scope of practice and being supervised by proper personnel. Develop a formalized written process for validating the credentials of all licensed and certified professionals and include written job descriptions for all staff with patient care responsibilities. Consider developing a procedure or protocol to annually assess the continued competency of all staff who perform procedures.
- Document thoroughly and accurately. Documentation is the best evidence of the care that was provided to a patient. Accordingly, thoroughly document all findings and discussions you have with a patient—especially informed consent discussions. In some instances, late entries, addendums, and corrections may be necessary to ensure accuracy and continuity of care. When an amendment is necessary, include a clarification note as soon as possible after the original entry; state the reason for the change and the current date and time. Never obliterate or obscure an entry to amend it.
- Create a culture of safety. Practices with leaders who promote a culture of safety and empower staff to speak up about safety issues are less vulnerable to patient safety risks. Leadership should be dedicated to building teams that exhibit trust, respect, and a commitment to patient safety. Empower and encourage staff to speak up if they see anything that causes worry or concern at any point during a visit or procedure. Foster a culture of safety by encouraging practitioners to pause to reassess the clinical situation and provide feedback to the team when patient safety issues are brought to their attention.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.