
August • 24 • 2023
Best Practices for Patient Discharge to Avoid Escalation and Liability
Summary
When patient discharge is necessary, best practices can help providers avoid escalation and reduce practitioner liability.
Healthcare practitioners and facilities may occasionally need to terminate a patient from their care. Because these situations can be difficult, many providers seek guidance from their attorney or risk manager. In fact, the most frequent calls to the Coverys Risk Management Consultation Line involved questions related to discharging patients with the second-most common reason related to safety, security, and potential workplace violence.
To avoid unnecessary conflict and liability exposures, it’s important to carefully follow best practice guidelines, keeping in mind that discharging a patient is a process that should only be undertaken after all other possible interventions have failed.
Liability Exposures
Even when you follow best practices, patient discharge can lead to allegations of abandonment or discrimination. Papers published in the National Institutes of Health National Library of Medicine provide the following definitions:
- Abandonment is “a breach of duty and is defined as unilateral termination of the physician-patient relationship without providing adequate notice for the patient to obtain substitute medical care.”
- Discrimination is defined as “negative actions or lack of consideration given to an individual or group that occurs because of a preconceived and unjustified opinion.”
Accusations of abandonment can result in civil liability, particularly if the discharge occurs without good reason or without sufficient notice, leaving the patient unable to find another practitioner.
Patients may sue practitioners for abandonment or discrimination if the discharge results in harm, neglect, or injury—even if the discrimination was unintentional. Other possible consequences are licensure discipline and even criminal prosecution as well as reputational and financial harm.
Workplace Violence Exposures
In extreme cases, a discharge may even trigger a violent reaction. Violent incidents may also be the reason for discharge.
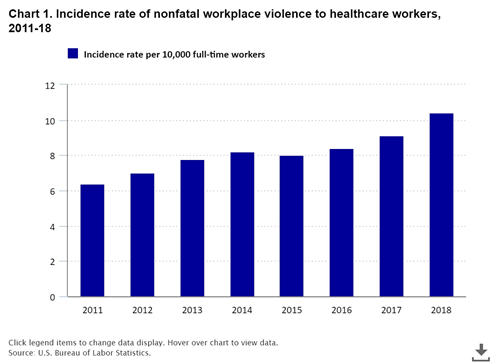
Healthcare workers experience workplace violence more often than most other industries. The U.S. Bureau of Labor Statistics (BLS) tracks workplace homicides and nonfatal injuries that result from an intentional injury by another person. BLS data shows that people in the healthcare and social service industries are five times more likely to suffer a workplace violence injury compared to the average for workers in all industries. According to an article in National Library of Medicine, patients have been identified as the most common committers of this violence.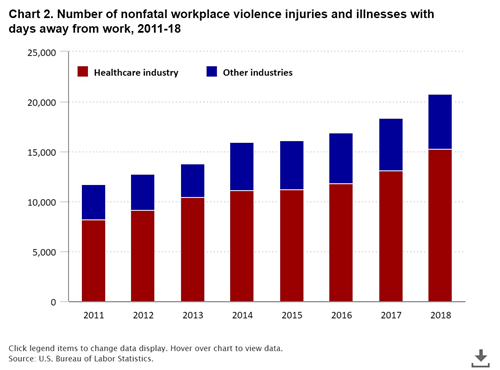
BLS data from 2011 to 2018 shows that workplace violence in healthcare settings is on the rise. In 2011, the rate of nonfatal incidents per 10,000 full-time workers was 6.4. By 2018, the rate had increased to 10.4 per 10,000 compared to the all-worker incidence rate of 2.1. In psychiatric and substance abuse hospitals, the rate was 124.9 per 10,000. Workers in the healthcare and social services industries are five times more likely to suffer a workplace violence injury than workers overall.
The Department of Labor recommends having a workplace violence program in place to prevent incidents. This involves defining three levels of violence. Level one is when a person is intimidating, disrespectful, uncooperative, or verbally abusive. Practitioners should report and document such behavior. If behavior escalates to threat of physical harm or greater, it may be necessary to call 911 or take other steps to secure the safety of workers and others.
In some cases, de-escalation techniques may prevent incidents from developing into violence. The Crisis Prevention Institute recommends 10 techniques:
- Be empathetic and nonjudgmental.
- Respect personal space.
- Use nonthreatening nonverbals, such as gestures and tone of voice.
- Keep your emotional brain in check and stay calm, rational, and professional.
- Focus on how the person feels.
- Ignore questions that challenge your authority.
- Set limits.
- Choose what you insist on wisely.
- Allow silence for reflection.
- Allow time for decisions.
When Is It Acceptable to Discharge a Patient?
Patients should never be terminated due to their gender, race, religion, or sexual orientation. Additionally, providers should not terminate a patient who is in crisis, and they should use extreme caution when terminating surgical, pregnant, or behavioral health patients.
That being said, there may be acceptable reasons for termination, such as when the patient:
- Repeatedly cancels follow-up visits or fails to keep scheduled appointments.
- Does not adhere to prescription refill or treatment plans.
- Is rude, uses disparaging language, sexually harasses others, makes verbal threats, or jeopardizes the safety of others.
- Brings firearms or weapons.
- Has a backlog of unpaid bills.
Risk Mitigation Techniques
Termination of the practitioner-patient relationship is a process and not an event to be taken lightly. It should be viewed as the last option after exhausting all other possible interventions. Part of the process involves proactive risk mitigation techniques to head off potential problems and swiftly address conflicts when they arise. Best practices include:
- Set clear expectations from the beginning. Patients and healthcare providers need to know what you expect of them. Use clear signage in the waiting area and patient care rooms and include behavior expectations in patient-practitioner care agreements.
- Remind the patient of your expectations and point out any behavior that fails to meet expectations. It can be helpful to have phrases ready, for example, “We don’t tolerate that kind of speech here.”
- Investigate contributory reasons. When friction occurs and behavior escalates, look for the root causes of the problems with empathy and a lack of judgement. For example, is the patient grieving the death of a loved one or battling financial problems? Are language or culture barriers interfering with good communication? Does the patient lack the health literacy or mental competency to follow instructions?
- Educate staff on how to manage disruptive behavior. This training is important for everyone on the healthcare team, including office support staff.
- Give formal notice when a patient is at risk of termination. Don’t let termination come as a surprise. Explain that termination is the next step if things don’t improve and explain exactly what could cause termination.
- Consider discharge if the behavior continues or escalates. Assess each case on an individual basis. It’s also important to check health plan contracts and comply with state regulations. Resolve acute conditions before termination and consult with an attorney if you have any questions.
- Document everything. You need to document every instance of escalated behavior, even if you don’t think it will result in termination. Also document the attempted interventions and the patient’s response. Go into detail.
An immediate discharge may be necessary for criminal or egregious acts, such as physical violence, threats of physical violence, stalking, or criminal activity that involves the practice. However, you should use caution when discharging a long-term patient over uncharacteristic violent behavior or verbal abuse. Try to identify the reason for the change in behavior before resorting to termination.
Risk Recommendations for Discharging a Patient
Following are steps to take once the decision has been made to discharge a patient.
- Have a conversation with the patient. Let the patient know you have reached the point of termination to avoid this information coming as a surprise.
- Send a certified letter. This step is important for documentation. Send the letter to the patient’s home address and request a return receipt. File a copy in the patient’s record. You can scan the letter to add it to the patient’s electronic medical records. If the letter is returned, file the returned letter and then mail a duplicate letter in a plain envelope without a return address.
- In the letter, include the effective date of termination and available resources, such as a local medical center. Provide a reasonable time frame to ensure the patient can find another provider, for example, 30 days for emergency care. Also state exactly which relationship you are terminating—is it with the provider or the entire practice?
- If the patient won’t leave or there is a safety concern, contact security or law enforcement to escort the patient off the premises. Enlist help in de-escalating any potential violence.
Discharging a patient is never easy. Following the best practices outlined above can help you proceed confidently and reduce potential exposures.
This article is based in part on “Discharge from Practice: Keeping You and Your Patient Safe,” presented by Kerri Aramini, MJ, BSN, RN, CPHRM, CLNC, and Ronnie Hanson, BSN, MHA, RN, CPPS, CHPHRM .
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.